Recently I had the opportunity to be a guest speaker for a Master-level class at Kent State University’s College of Architectural and Environmental Design. The class was part of their Healthcare Master of Architecture program, and focused on Hospital Acquired Infections (HAI) and the physical environment. Over my 20 years of professional practice, 14 of which have been dedicated to healthcare, infection control protocol has become increasingly more important.
A simple definition for HAI is any infection that was not present or incubating prior to an admission to a hospital or healthcare setting, but occurs within 48 hours after admission. These types of infections are not only difficult to treat and identify, but also have become a prominent topic due to the large number of annual deaths attributed to them, as well as the billions of dollars of direct cost to health systems.
HAIs have a broad range of types, including gastrointestinal, urinary tract and those found in the bloodstream. A major contributor to the spike in HAI cases over the past several years is an overuse of antibiotics. This much published overuse creates highly resistant “superbugs,” which, at the very least, are extremely difficult to treat, and can quickly become life threatening.
Like an infection, the HAI problem has spread from the hospital into ambulatory settings. With healthcare reform and the need for cost reduction, health systems are completing more procedures outside the inpatient setting. The problem is that outpatient facilities may not have the same level of infection control design required within the hospital.
As designers, we can help by creating a design that enables the practice of proper protocols instead of inhibiting them. Designers need to become students of infection control best practices and use our knowledge of space utilization to encourage good provider infection prevention techniques such as the ones listed below.
Hand Washing
A generally understood best practice to decrease infection transmission, including HAI, is proper hand washing. Locating a hand-washing sink within the natural path of staff will encourage use of the sink; otherwise, staff may be less inclined to use the sink during high-stress circumstances.
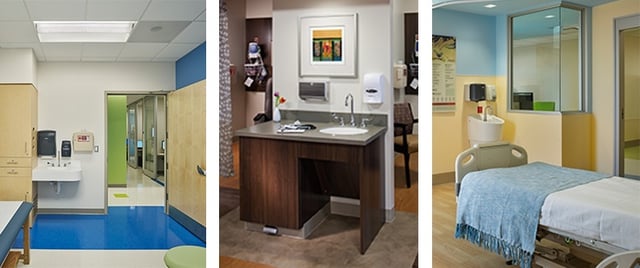
To understand the natural path of travel, the designer needs to understand fully the facility’s operations and flow. Working with staff to design a LEAN workflow creates a more efficient, less stressful environment in which staff are encouraged to wash their hands at certain junctures throughout their tasks. Building mock-ups early in the design process allows staff to test the space and properly develop the environment to comply with infection control guidelines.
“God is in the details.”
Creating a room that has multiple finishes, each with their own cleaning requirements doesn’t lend itself for proper sanitation. Minimizing the types of surfaces in any space is better for maintaining the proper level of cleanliness since bacteria will take full advantage of any space on which it can remain. Manufacturers regularly introduce new products developed specifically for infection control. Our job as designers includes keeping current with industry standards to ensure we use the best materials available. Consider, for instance, antimicrobial finishes on the surfaces of “high touch” areas. Natural finishes are better than coatings as they don’t wear out with use.
Additionally, reducing the number of seams can be key. As designers, we should take advantage of the opportunity for a seamless joint between two materials as appropriate in the space.
Phasing and Infection Control Risk Assessments
In addition to developing a best practice design, the team must work closely with the hospital and contractor to confirm the Infection Control Risk Assessment (ICRA) is fully coordinated during construction. The team is required to meet with the Infection Control Department and understand the hospital’s protocol since every health system has their own ICRA standards. Understanding the hospital’s ICRA requirements influences the design, and the team must review those requirements early in the process. Understanding how the ICRA plan affects the design will also provide an outline for detailing the construction-phasing plan.
 Since hospitals operate 24/7, most projects undergo construction while the facility maintains adjacent operations. Detailed meetings with all stakeholders should address construction boundaries as well as temporary operations when the standard workflow pathways are interrupted. For most renovations, the contractor has to move both demolished and new material through active areas of the hospital. From the start of the project, the team must establish and maintain open lines of communication with the Infection Control Department for the duration.
Since hospitals operate 24/7, most projects undergo construction while the facility maintains adjacent operations. Detailed meetings with all stakeholders should address construction boundaries as well as temporary operations when the standard workflow pathways are interrupted. For most renovations, the contractor has to move both demolished and new material through active areas of the hospital. From the start of the project, the team must establish and maintain open lines of communication with the Infection Control Department for the duration.
Just as HAIs influence multiple facets of healthcare, designers need to elevate their knowledge and allow infection control best practices to influence them from the early planning stages down to the specifics of airflow within an operating room. When designers are armed with this knowledge, the design will help decrease transmission of deadly HAIs for the life of the space.
This post was written by former Array employee, Dwight Young.

